Is It Safe To Buy Eliquis From A Canadian Online Pharmacy?

If you’re among the millions of Americans struggling to afford Eliquis, you’re facing an impossible choice: pay hundreds of dollars each month for a medication that prevents life-threatening blood clots, or risk your health by skipping doses or discontinuing treatment altogether. Eliquis (apixaban) has become one of the most commonly prescribed anticoagulants in the United States, yet its price remains out of reach for many patients, even with insurance coverage.
This article examines whether purchasing Eliquis from Canada is safe, legal, and practical for Americans seeking affordable access to this essential medication. Understanding your options matters because medication non-adherence due to cost can lead to serious health consequences, including stroke and pulmonary embolism.
Drawing on FDA guidance, pharmaceutical supply chain data, and information from certified pharmacy organizations, we’ll explore the development and availability of Eliquis, the legal landscape surrounding cross-border medication purchases, how to identify legitimate Canadian pharmacies, and the substantial cost savings available through CIPA-certified sources like MedicationsCanada.com.
What is Eliquis?
Eliquis (apixaban) is a prescription anticoagulant used to lower the risk of stroke and blood clots in patients with atrial fibrillation (AFib), deep vein thrombosis (DVT), or pulmonary embolism (PE).
Brand Eliquis
Eliquis, an anticoagulant, was developed jointly by Pfizer and Bristol-Myers Squibb starting in 2007. The medication received U.S. approval in December 2012. By 2023, Eliquis had become the 28th most frequently prescribed drug in the United States, with over 19 million prescriptions written.
Generic Eliquis
While a generic version of Eliquis (apixaban) was approved by the FDA in 2019, patent litigation has delayed its wide availability in the U.S.
Generic versions are available in several other countries, including Canada, at a much lower cost. The FDA’s Abbreviated New Drug Application (ANDA: 210128) confirms that approved generics contain the same active ingredients, strength, dosage form, and route of administration as the brand-name drug and must meet the same standards for quality and efficacy.
The U.S. Food and Drug Administration said on Monday it has approved the first generic version of Bristol-Myers Squibb Co and Pfizer Inc’s blood thinner Eliquis. The approval was granted to Micro Labs Ltd and Mylan Pharmaceuticals Inc, the agency said.” (Reuters News December 23, 2019)
The availability of generic medications raises an important question about pharmaceutical supply chains: regardless of whether a medication is brand-name or generic, where do the active pharmaceutical ingredients actually come from? Understanding the source of these ingredients is crucial for patients concerned about drug quality, safety, and the factors that influence medication costs in the United States.
Where are the active ingredients for medications sold in the U.S. obtained?
Information about the U.S. prescription drug supply chain remains fragmented and inconsistent, suggesting that no single entity has a complete understanding of drug sourcing.
According to a 2012 USA Today article, approximately 80 percent of the active pharmaceutical ingredients (APIs) and 40 percent of finished medications come from outside the United States, primarily from countries like India and China. This means that even the U.S. sold medications often rely on a global supply chain for their production. U.S. sold Eliquis
Is it against the law to order medications from outside the USA?
About five million Americans buy medication internationally each year because of high costs in the United States. – New York Times, March 24, 2014, by Op-Ed Contributor Gabriel Levitt
The FDA explains that it “typically does not object to personal imports of drugs that FDA has not approved under certain circumstances.” They also publish guidance for the personal importation of drug or device products.
If you’re considering purchasing Eliquis or its generic form (apixaban) from Canada or other countries, you may wonder about the legality. Under federal law, importing prescription medications for personal use is generally prohibited, yet millions of Americans continue to do so each year. This creates a regulatory gray area where enforcement remains inconsistent and politically contentious.
In practice, the FDA typically exercises discretion and allows shipments that meet certain criteria: the medication must be for personal use, prescribed by a licensed physician, and limited to a 90-day supply or less. Statistics show that fewer than 1% of prescription drug orders are intercepted at the border.
Additionally, several states have explored or implemented their own prescription importation programs, and some lawmakers have advocated for federal reforms to make Canadian drug importation officially legal, though comprehensive legislation has yet to pass. In February 2021, H.R. Bill 832 was introduced in the House of Representatives with the goal of amending the Federal Food, Drug, and Cosmetic Act to permit personal importation of safe and affordable medications from approved Canadian pharmacies. However, as of 2025, this legislation remains stalled and has not been enacted into law.
How does one safely purchase medications from Canadian online pharmacies?
When considering purchasing medications from Canada, it’s essential to verify that you’re working with a legitimate, regulated pharmacy. The Canadian International Pharmacy Association (CIPA) serves as a vital resource for patients seeking safe access to Canadian medications. Established in 2002, CIPA is a non-profit organization that certifies and monitors online pharmacies operating in Canada. CIPA-approved pharmacies must meet rigorous standards, including proper licensing in their Canadian province, employing licensed pharmacists to review all prescriptions, sourcing medications exclusively from approved manufacturers, and maintaining secure handling of patient information and medication shipments.
For Americans seeking a trusted option, MedicationsCanada.com stands out as an active CIPA member with a proven track record. As a CIPA-certified member, MedicationsCanada.com adheres to all Canadian regulatory requirements and provides you with access to both brand-name Eliquis and its generic equivalent, apixaban, at significantly reduced prices compared to U.S. retail costs.
You can buy brand-name 5mg Eliquis for about $1 per pill online from MedicationsCanada.com.
Our platform offers straightforward ordering processes, requires valid prescriptions from licensed healthcare providers, and ships medications directly to your homes. Our team is available to answer questions about medications, potential interactions, and proper usage, providing an additional layer of safety and support for you navigating your treatment options.
Call us toll-free on +1-866-481-5817 or email info@medicationscanada.com.
Comparing the Cost of Eliquis: U.S. vs. Canadian Pharmacies
Eliquis Prices in the United States
According to data from the National Institutes of Health (NIH) and GoodRx, a 30-day supply of brand-name Eliquis 5mg (60 tablets) costs between $550 and $650 without insurance at U.S. retail pharmacies. Even with insurance coverage or discount cards, patients often pay around $450 or more—a price point that remains financially burdensome for many Americans managing chronic conditions.
Eliquis Through Canadian Pharmacies
In contrast, the same 30-day supply of brand-name Eliquis 5mg (60 tablets) purchased through MedicationsCanada.com costs approximately $120 to $150 USD. This represents a potential savings of up to 75% compared to U.S. retail prices, making long-term anticoagulation therapy significantly more affordable for patients who pay out of pocket or face high deductibles.
Generic Apixaban: Even Greater Savings
For those seeking additional cost reduction, generic apixaban available through Canadian pharmacies offers an even more economical option. A 30-day supply of generic apixaban 5mg typically costs between $70 and $90 USD. As an FDA-equivalent generic, it contains the same active ingredient and meets identical standards for safety and efficacy as the brand-name medication, providing therapeutic benefits at a fraction of the cost.
Conclusion
The stark price difference between U.S. and Canadian pharmacies reveals why millions of Americans turn to cross-border medication purchases each year. While Eliquis can cost $550 to $650 per month in the United States, the same brand-name medication is available through CIPA-certified Canadian pharmacies for as little as $120 to $150, with generic apixaban offering even greater savings at $70 to $90 per month. These savings can transform medication adherence from an impossible burden into a manageable reality, potentially preventing the devastating health consequences that occur when patients ration or discontinue anticoagulation therapy due to cost. If you’re considering this option, start by verifying that any pharmacy you consider is CIPA-certified and requires a valid prescription from your healthcare provider.
Contact MedicationsCanada.com at +1-866-481-5817 or info@medicationscanada.com to discuss your options with licensed pharmacists who can guide you through the ordering process. Ensure your shipments don’t exceed a 90-day supply for personal use, and maintain open communication with your prescribing physician about your treatment plan. Taking control of your medication costs doesn’t mean compromising on safety—it means making informed choices that support both your health and financial wellbeing.
References
- Orange Book. Accessdata.Fda.Gov. 2025
- Atrial Fibrillation. Cdc.Gov. 2023
- Stroke Prevention In Atrial Fibrillation. Heart.Org. 2022
- Eliquis Medication Guide. Pfizer.Com. 2022 FDA Approves Eliquis. Fda.Gov. 2012
- Pharmaceutical Sales Report. Statista.Com. 2023
- FDA Approves First Generics Of Eliquis. Fda.Gov. 2019
- Generic Drug Facts. Fda.Gov. 2021
- Safeguarding Pharmaceutical Supply Chains. Fda.Gov. 2020
- Personal Importation Policy. Fda.Gov. 2022
- Importation Of Prescription Drugs. Fda.Gov. 2022
- Safe Importation Action Plan. Hhs.Gov. 2020
- KFF Health Tracking Poll. Kff.Org. 2019
- Affordable And Safe Prescription Drug Importation Act. Congress.Gov. 2023
- State Prescription Drug Importation Programs. Ncsl.Org. 2023
- Prescription Drug Pricing Report. Goodrx.Com. 2023
- Medicare Prescription Drug Coverage Report. Medicare.Gov. 2023
- International Medication Price Comparison. Medicationscanada.Com. 2023
- Generic Medication Pricing. Medicationscanada.Com. 2023
- Three Times As Many People Have Atrial Fibrillation Than Previously Known. Harvard Medical School. 2024
- How Many People Have A-Fib? Three Times More Than We Thought. University Of California San Francisco. 2024
Blood Thinner Vegetables and Fruits: Natural Foods to Support Healthy Circulation

Ever worry about blood clots or sluggish circulation? While prescription blood thinners play a vital role for many people, not everyone realizes that everyday foods, especially certain vegetables and fruits, can gently support healthy blood flow. These natural options don’t replace medication, but research shows they may help platelets stay less “sticky,” reduce inflammation, and protect blood vessels.
Understanding how natural blood thinners, vegetables, and fruits work matters because circulation affects everything from heart health to energy levels. That’s why this guide explores the top foods with blood-thinning properties, from garlic and onions to berries and grapes. You’ll also learn about nutrients and enzymes that keep blood moving smoothly, lifestyle tips for safe balance, and when to check in with your doctor. By the end, you’ll know how to use everyday foods to support your heart and circulation better, safely, and naturally.
Even with the use of existing anti-clotting therapies, such as aspirin, clopidogrel (Plavix), and warfarin (Coumadin), each year there are approximately 400,000 recurrent episodes among patients who previously experienced a stroke or heart attack – Robert Flaumenhaft, Professor of Medicine, Beth Israel Deaconess Medical Center.
How Natural Blood Thinners Work
Researchers have discovered that rutin, a natural compound abundant in many fruits and vegetables, demonstrates significant potential in preventing dangerous blood clots. The groundbreaking study, conducted by scientists at Beth Israel Deaconess Medical Center (BIDMC), a Harvard Medical School affiliate, successfully demonstrated rutin’s ability to block clot formation in laboratory models of thrombosis.
These natural blood-thinning effects come from four main types of compounds found in everyday foods: salicylates, flavonoids, omega-3 fatty acids, and enzymes.
Salicylates
Salicylates are a group of natural chemicals found in plants that act as a defense against pests and pathogens. Salicylic acid (SA) is present in plant foods such as fruits, vegetables, spices, etc. People eating a vegetarian diet tend to have higher concentrations of salicylic acid circulating in their bloodstream compared to people who eat meat. This happens because salicylic acid occurs naturally in many plant foods – especially fruits, vegetables, herbs, and spices. Since vegetarians eat more of these plant-based foods, they consume more natural salicylic acid through their diet.
The amount of salicylic acid that vegetarians excrete in their urine can be similar to what you’d see in people taking small, daily doses of aspirin. This is significant because aspirin is actually acetylsalicylic acid, which the body converts to salicylic acid.
Flavonoids
Flavonoids, a group of natural substances, are found in fruits, vegetables, grains, bark, roots, stems, flowers, tea, and wine. These natural products are well known for their beneficial effects on health, and efforts are being made to isolate the ingredients, so-called flavonoids. Flavonoids are now considered an indispensable component in a variety of nutraceutical, pharmaceutical, medicinal, and cosmetic applications.
Omega-3 Fatty Acids & Vitamin E
Omega-3 fatty acids are found in foods such as fish and flaxseed. It is also found in plant oils such as soybean, chia seeds, walnuts, and canola oils. Omega-3 fatty acids reduce one clotting pathway and may interfere with thrombin generation and adhesion, thus altering clot-promoting chemicals.
Vitamin E, a powerful antioxidant, also plays a role. It slows platelet clumping and, in higher doses, can affect clotting factors that depend on vitamin K.
Enzymes (Nattokinase)
Nattokinase, an enzyme from fermented soy, is especially powerful; it helps dissolve clots and supports your body’s natural way of keeping blood vessels clear. These enzymes may promote heart health without some of the stronger side effects that prescription blood thinners can bring.
Green Vegetables Blood Thinner: Science-Backed Leafy Greens That Affect Blood Clotting
Garlic
Garlic is a natural blood thinner because it stops blood platelets from sticking together, which lowers the chance of clots forming. This effect comes from a sulfur compound in garlic called ajoene. Garlic can also make blood-thinning medicines work stronger, which may help protect heart health.
Onion
Onions can help thin the blood because it has antioxidants and compounds that stop clots from forming. Research shows that onion extracts may lower cholesterol and improve blood fat levels, which supports heart health. They also contain quercetin, a plant compound that prevents platelets from clumping, allowing blood to flow more smoothly.
Tomatoes
Tomatoes have natural compounds that stop platelets from clumping together, which lowers the risk of blood clots. Studies show that tomato extracts may help reduce platelet activity, lower blood pressure, and improve cholesterol levels. This supports better blood flow and overall heart health.
Broccoli
Broccoli contains natural compounds like sulforaphane that may help lower the risk of harmful blood clots. It’s also packed with antioxidants and fiber, which reduce inflammation and support healthy cholesterol levels, protecting the heart. But since broccoli is high in vitamin K, people taking blood thinners should eat it in consistent amounts to avoid interfering with their medication.
Kale
Kale is loaded with antioxidants like quercetin and kaempferol, which fight inflammation and support heart health.
Brussels sprouts
Brussels sprouts can influence blood clotting because they speed up how the body processes warfarin, which may affect its effectiveness. They’re also rich in antioxidants and fiber that help lower inflammation and support heart health. However, since they are high in vitamin K, people on blood thinners should keep their intake steady and monitor it carefully.
Cauliflower
Cauliflower is rich in antioxidants and fiber, which support good digestion and healthy blood circulation. Since it contains vitamin K, people taking blood thinners should eat it in moderate, consistent amounts.
Cabbage
Cabbage is rich in antioxidants, vitamin C, and fiber that help reduce “bad” cholesterol and improve blood vessel health. These properties support better blood circulation and may lower blood pressure, contributing to heart disease risk reduction.
Artichoke
Artichoke is rich in antioxidants and plant nutrients that protect blood vessels. These compounds may help blood flow smoothly and lower the risks linked with clotting.
Chicory
Chicory leaf compounds reduce platelet activity, making blood less likely to clot too quickly. It also contains antioxidants that protect blood vessels and support smoother circulation.
Which Fruit is Best for Blood Thinners?
Blueberries
Blueberries are packed with natural plant compounds like anthocyanins and polyphenols that support healthy blood flow. Research in people shows that eating berries can make platelets less sticky, lowering clot formation by about 11% compared to those who didn’t eat them. This makes blueberries a great natural blood thinner.
Strawberries
Strawberries are rich in flavonoids and anthocyanins that keep blood vessels healthy and help prevent platelets from clumping together. Studies on berry intake show that people who eat them have lower platelet activity, which points to a gentle, natural blood-thinning effect.
Cranberries
Cranberries contain special compounds called proanthocyanidins that may work in a way similar to aspirin, helping slow down platelet activity. In fact, a medical case once linked cranberry intake with extra bleeding during surgery, showing its potential blood-thinning effect.
Grapes
Grapes and grape juice are rich in polyphenols like resveratrol, which support heart health and help prevent platelets from sticking together. Research on supplements and diet reviews highlights grapes as one of the fruits with proven natural antiplatelet benefits.
Cherries
Sour cherries are full of anthocyanins and flavonoids that promote healthy circulation by reducing platelet clumping. In a human study, sour cherry intake lowered platelet activity by about 40% within just a few hours, showing a quick and powerful effect.
Oranges
Oranges are loaded with vitamin C and plant compounds like hesperidin that keep blood vessels strong and may slightly reduce platelet stickiness. Reviews on citrus fruits often highlight their role in supporting heart health and offering mild natural blood-thinning benefits.
Lifestyle & Supplement Considerations
When you take blood thinners, making specific lifestyle adjustments is essential to stay safe and ensure your medication works effectively. Blood thinners help prevent harmful clots but also increase your risk of bleeding, so you need to manage diet, activities, and supplements carefully.
Following consistent habits and consulting your healthcare provider about changes can greatly reduce complications.
Keep Vitamin K Intake Consistent
Foods high in vitamin K (like kale, spinach, broccoli) can affect medications such as warfarin. It is important to maintain a consistent amount daily rather than avoid these foods entirely.
- Avoid certain herbal supplements and natural products
- Limit alcohol consumption
- Exercise caution to prevent injuries
- Communicate regularly with your healthcare provider
When to Consult Your Healthcare Provider
Blood thinners help prevent dangerous blood clots but carry a risk of serious bleeding. It is important to know when to contact a healthcare provider while taking blood thinners, whether these are medications or influenced by diet.
- Seek immediate medical help for signs of serious bleeding, such as unusual bruising, prolonged bleeding, red or brown urine, black or bloody stools, or vomiting blood.
- Call if experiencing severe headache, dizziness, weakness, or unexplained pain, especially after a fall or head injury.
- Report any new medications, supplements, or dietary changes to your provider, as these can affect blood thinner effectiveness.
- Notify your provider if you have any questions or concerns about symptoms, medication dosing, or side effects.
- Regular blood tests and follow-up appointments are essential for safe management.
This cautious approach prevents complications and ensures safe treatment.
Frequently Asked Questions
Can I eat blood-thinning foods if I’m not on medication?
Yes, incorporating natural blood-thinning foods into your diet is generally safe and beneficial for most people. These foods support overall cardiovascular health through their anti-inflammatory and antioxidant properties.
How quickly do natural blood thinners work?
Unlike medications that work within hours, natural blood-thinning foods provide gradual benefits over weeks to months of consistent consumption. Their effects build up slowly as part of your overall dietary pattern.
Should I avoid vitamin K completely if I’m on warfarin?
No, complete avoidance isn’t necessary or recommended. Maintaining consistent vitamin K intake allows your healthcare provider to optimize your medication dose while ensuring you get important nutrients from leafy greens and other vegetables.
Can I drink green tea while taking blood thinners?
Green tea contains vitamin K and natural compounds that may affect blood clotting. Moderate, consistent consumption is usually fine, but discuss your tea consumption with your healthcare provider, especially if you drink large amounts.
Are frozen fruits and vegetables as effective as fresh ones?
Frozen fruits and vegetables retain most of their beneficial compounds and can be just as effective as fresh options. However, avoid products with added sugars or sodium that might counteract the cardiovascular benefits.
Conclusion
What you eat every day can quietly make a big difference in how smoothly your blood flows. The vegetables and fruits we’ve explored, like garlic, berries, and leafy greens, don’t replace medication, but they can give your heart and blood vessels steady support.
Why does that matter? Because good circulation fuels everything from your energy to your long-term heart health. Choosing foods that keep platelets less sticky and protect blood vessels is a simple way to care for yourself in the long run.
You don’t need to make big changes all at once. Start small, add an extra serving of veggies to dinner, reach for fresh fruit as a snack, or try a new spice in your cooking. And if the cost of blood thinner medication is a concern, exploring trusted pharmacies like Medications Canada can help you access safe, affordable options. Little steps like these support both your health and your budget.
While nutrient-rich foods support your circulation naturally, many people also need prescription blood thinners to manage specific health conditions. If you’ve been prescribed medications like Eliquis, Xarelto, Warfarin, Pradaxa, Heparin, Lovenox, Plavix, or Brilinta, managing your prescription costs is an important part of your health journey.
Medications Canada offers Americans access to these essential medications through licensed Canadian pharmacies—at significantly lower prices and with no dispensing fees. Whether you’re taking Eliquis for atrial fibrillation, Xarelto to prevent blood clots, Warfarin for long-term anticoagulation, Pradaxa as a newer oral anticoagulant, Heparin or Lovenox for injectable options, or antiplatelet medications like Plavix and Brilinta to prevent heart attacks and strokes, Medications Canada provides a trusted, affordable solution.
Visit Medications Canada today to learn more about how you can save on your blood thinner prescriptions while maintaining the quality care you deserve.
References
- National Library of Medicine. (2025). Trends in Oral Anticoagulant Use and Individual Expenditures Across the United States from 2014–2020
- National Library of Medicine. (2021). The Impact of Diet and Exercise on Drug Responses
- National Library of Medicine. (2024). Functional Foods in Preventing Human Blood Platelet Hyperactivity-Mediated Diseases—An Updated Review
- National Library of Medicine. (2024). The Circulatory System and Oxygen Transport
- National Library of Medicine. (2025). Therapeutic applications of natural products in the management of venous diseases: a comprehensive review
- National Library of Medicine. (2003). Dietary salicylates
- National Library of Medicine. (1969). The influence of salicylate on platelets and whole blood adenine nucleotides
- National Library of Medicine. (2020). The Effects of Flavonoids in Cardiovascular Diseases
- National Library of Medicine. (2024). Antiplatelet Effects of Flavonoid Aglycones Are Mediated by Activation of Cyclic Nucleotide-Dependent Protein Kinases
- National Library of Medicine. (2020). Important Flavonoids and Their Role as a Therapeutic Agent
- National Library of Medicine. (2015). Commonly Used Dietary Supplements on Coagulation Function during Surgery
- National Library of Medicine. (2015). 5 Things To Know About Omega-3s for Heart Disease
- National Library of Medicine. (2017). Nattokinase: An Oral Antithrombotic Agent for the Prevention of Cardiovascular Disease
- National Library of Medicine. (2018). Nattokinase: A Promising Alternative in Prevention and Treatment of Cardiovascular Diseases
- National Library of Medicine. (1993). Effects of a garlic-derived principle (ajoene) on aggregation and arachidonic acid metabolism in human blood platelets
- National Library of Medicine. (2016). Review on mechanisms and interactions in concomitant use of herbs and warfarin therapy
- National Library of Medicine. (2021). The effects of Allium cepa L. (onion) and its active constituents on metabolic syndrome: A review
- National Library of Medicine. (2022). Scientific Evidence of the Beneficial Effects of Tomato Products on Cardiovascular Disease and Platelet Aggregation
- National Library of Medicine. (2014). Antithrombotic activities of sulforaphane via inhibiting platelet aggregation and FIIa/FXa
- National Library of Medicine. (2023). Broccoli: A Multi-Faceted Vegetable for Health: An In-Depth Review of Its Nutritional Attributes, Antimicrobial Abilities, and Anti-inflammatory Properties
- Mayo Clinic. (2024). Warfarin diet: What foods should I avoid?
- National Library of Medicine. (2023). Antioxidant and Antiproliferative Activities of Kale (Brassica oleracea L. Var. acephala DC.) and Wild Cabbage (Brassica incana Ten.) Polyphenolic Extracts
- BPS Journals. (2020). Warfarin and food, herbal or dietary supplement interactions: A systematic review
- National Library of Medicine. (2022). Cruciferous Vegetables and Their Bioactive Metabolites: from Prevention to Novel Therapies of Colorectal Cancer
- Medical News Today. (2017). Everything you need to know about cauliflower
- National Library of Medicine. (2016). Assessment of bioactive metabolites and hypolipidemic effect of polyphenolic-rich red cabbage extract
- National Library of Medicine. (2023). Phytochemicals, Nutrition, Metabolism, Bioavailability, and Health Benefits in Lettuce—A Comprehensive Review
- National Library of Medicine. (2021). Preparations from selected cucurbit vegetables as antiplatelet agents
- MDPI. (2022). A Review of the Effect of Preparations from Vegetables of the Asteraceae Family and Cucurbitaceae Family on the Cardiovascular System and Its Diseases
- MDPI. (2021). Potential Health Benefits of Plant Food-Derived Bioactive Components: An Overview
- Science Direct. (2022). The in vitro antiplatelet activities of plant extracts from the Asteraceae family
- National Library of Medicine. (2008). Favorable effects of berry consumption on platelet function, blood pressure, and HDL cholesterol
- National Library of Medicine. (2013). Cranberries and Their Bioactive Constituents in Human Health
- AHA.Journals. (2010). Nutrition, Supplements, and Vitamins in Platelet Function and Bleeding
- Research Gate. (2024). Effects of sour cherry fruits on platelet aggregation and arterial blood pressure
- National Library of Medicine. (2020). Effects of chronic consumption of specific fruit (berries, citrus, and cherries) on CVD risk factors: a systematic review and meta-analysis of randomised controlled trials
- Science Direct. (2021). Evidence for health properties of pomegranate juices and extracts beyond nutrition: A critical systematic review of human studies
- National Library of Medicine. (2022).
- National Library of Medicine. (2023). Does an apple a day keep away diseases? Evidence and mechanism of action
- MedlinePlus. (2024). Blood Thinners
- Cleveland Clinic. (2024). What To Avoid When Taking a Blood Thinner
- National Library of Medicine. (2024). Anticoagulation Safety
- National Library of Medicine. (2022). Platelet Aggregation Inhibition: An Evidence-Based Systematic Review on the Role of Herbs for Primary Prevention Based on Randomized Controlled Trials
- National Library of Medicine. (2000). Dietary antioxidants for cardiovascular prevention
- National Library of Medicine. (2023). Warfarin Drug Interactions
- National Library of Medicine. (2010). Beneficial effects of green tea: A literature review
- American Heart Association. (2023). Fresh, Frozen, or Canned Fruit and Vegetables: All Can Be Healthy Choices
- Oxford Academic. (2001). Salicylic acid: a link between aspirin, diet, and the prevention of colorectal cancer
Do Canadian Pharmacies Accept U.S. Prescriptions?

If you’re among the millions of Americans facing sticker shock at the pharmacy counter, you’ve likely wondered about this exact question. With prescription drug costs in the United States averaging more than double those in Canada, it’s no surprise that over 20 million Americans have either purchased medications from outside the U.S. or know someone who has. The good news is that yes, legitimate Canadian pharmacies can fill U.S. prescriptions through a well-established legal process called secondary medical review. However, navigating the world of cross-border pharmaceutical purchases requires understanding the regulations, safety considerations, and proper procedures to ensure you’re getting authentic medications from reputable sources.
This comprehensive guide will walk you through everything you need to know about using Canadian pharmacies safely and legally, from finding CIPA-certified providers to understanding the ordering process, insurance considerations, and quality standards that protect your health while saving you money.
How to Find Canadian Pharmacies That Fill U.S. Prescriptions
Finding trustworthy Canadian online pharmacies doesn’t have to be a daunting task filled with endless research and uncertainty. The Canadian International Pharmacy Association (CIPA) has already done the heavy lifting for consumers by establishing a comprehensive vetting system that makes identifying legitimate pharmacies remarkably straightforward.
CIPA serves as an independent watchdog organization that rigorously evaluates Canadian and international drugstores according to strict safety protocols. Their thorough assessment process examines multiple critical factors: drug authenticity and quality assurance, robust internet security practices to protect sensitive patient information, proper licensing and regulatory compliance, and adherence to professional pharmacy standards.
When pharmacies meet these demanding requirements, they earn a coveted spot on CIPA’s trusted pharmacy directory. The exclusivity of CIPA certification speaks volumes about its rigorous standards.
Out of hundreds of online Canadian pharmacies operating today, fewer than 80 have successfully met CIPA’s stringent criteria. This selective approval process means that when you see a pharmacy listed in CIPA’s directory, you can have confidence that they’ve committed to maintaining the highest standards of practice and safety for cross-border medication shipping.
Additional Considerations for Safe Online Pharmacy Shopping
Valid Prescriptions
Beyond CIPA certification, savvy consumers should also verify that their chosen pharmacy requires valid prescriptions from licensed healthcare providers, as legitimate pharmacies never sell prescription medications without proper authorization.
Contact information
Look for clear contact information, including a physical address and licensed pharmacist availability for consultation.
Unreal Prices
Additionally, be wary of prices that seem too good to be true, as extremely low costs can sometimes indicate counterfeit or expired medications. Finally, ensure the pharmacy uses secure, encrypted connections (look for “https” in the URL) when processing personal and payment information to protect your sensitive data throughout the transaction process.
What Happens When I Send My U.S. Prescription to a Canadian Pharmacy?
Canadian pharmaceutical regulations mandate that all prescriptions must be issued by healthcare professionals who are licensed to practice within Canada. This requirement naturally raises an important question: how can American patients legally obtain medications from Canadian pharmacies using prescriptions from their U.S. doctors?
The answer lies in a well-established process known as secondary medical review. When you submit a prescription from your American physician, reputable Canadian pharmacies facilitate a comprehensive evaluation by Canadian-licensed doctors. These qualified healthcare professionals thoroughly examine your U.S. prescription alongside your complete medical history and current health status. Following this detailed assessment, the Canadian physician will authorize and issue a new Canadian prescription when medically appropriate.
This secondary medical review process serves a dual purpose: it enables American patients to access more affordable medications from Canada while simultaneously providing an extra layer of medical oversight to enhance drug safety and therapeutic effectiveness. The system ensures that every prescription meets Canadian regulatory standards while maintaining the highest level of patient care and medication appropriateness.
Is It Common for Americans to Order Prescription Medications from Canada?
A 2021 study by Kaiser Family Foundation (KFF) indicated that roughly 20 million Americans reported buying, or knowing someone who buys, prescription drugs from outside the U.S. In 2023, the Campaign for Personal Prescription Importation stated that Americans received over 1 million prescriptions annually from online Canadian pharmacies. Though official numbers differ across various surveys and studies, the data consistently point to the same conclusion: a substantial number of Americans are looking north of the border for their prescription drugs, making Canada a go-to destination for affordable medications.
This widespread trend toward Canadian pharmacies is driven by one primary factor: significantly lower prescription drug prices. The cost savings can be substantial, with many Americans finding the same brand-name medications at a fraction of what they pay domestically.
Many Americans do order prescription medications from Canada, primarily to save money on high drug costs in the U.S. According to the Kaiser Family Foundation (KFF), people in the U.S. often pay much more for prescription drugs than in other developed countries, including Canada, where drug prices are about 44% of U.S. prices on average. This price difference motivates many Americans, especially seniors or those with financial struggles, to seek medications from Canadian pharmacies as a way to reduce their out-of-pocket expenses. Importing drugs from Canada is increasingly seen as a practical and cost-saving option, especially as states like Florida have received FDA approval to legally import certain prescription drugs from Canada to save on healthcare costs without compromising safety. While importing prescription drugs from Canada is not yet widespread nationwide, it is a positive strategy embraced by many Americans who need affordable medication.
Why Are Canadian Drug Prices Lower Than Prices in America?
When you understand the factors behind Canada’s lower prescription costs, you’ll see why the savings can be so significant for you as an American consumer. The Canadian government negotiates directly with pharmaceutical manufacturers to establish maximum allowable prices for prescription medications. The PMPRB regulates the pricing of patented medicines in Canada, ensuring prices remain within acceptable ranges compared to other developed countries. Canada’s patent system allows for earlier generic drug entry in many cases compared to the US market. Generic medications typically cost 20-90% less than brand-name equivalents, creating substantial savings opportunities. Unlike the United States, Canada prohibits direct-to-consumer pharmaceutical advertising. This restriction reduces marketing costs that pharmaceutical companies would otherwise pass on to consumers through higher drug prices.
Is It Safe to Buy U.S. Prescription Meds from Canadian Pharmacies?
Yes, it can be safe to buy U.S. prescription medications from legitimate Canadian pharmacies, but it requires careful due diligence to avoid serious risks. Both the U.S. Food and Drug Administration (FDA) and Health Canada warn against purchasing from unregulated online pharmacies. The primary risk is unknowingly buying from illegal, unverified websites that may sell counterfeit, expired, or improperly stored medication.
How to ensure safety
To minimize risks, always verify the legitimacy of an online pharmacy before purchasing.
- Check for licensing: Verify that the pharmacy is licensed by a provincial pharmacy regulatory authority (IPABC) in Canada
- Look for accreditation: Reputable online Canadian pharmacies are accredited by organizations like the Canadian International Pharmacy Association (CIPA).
- Require a valid prescription: Legitimate online pharmacies will require a valid prescription from a Canadian-licensed practitioner. These services often work with Canadian physicians to review and co-sign your U.S. prescription.
- Ensure clear contact information: A safe online pharmacy will provide a real Canadian street address, a phone number, and a way to contact a licensed pharmacist.
Are Drugs Sold Through Canadian Pharmacies the Same Quality as Those Sold in America?
Yes, for drugs from legitimate and licensed Canadian pharmacies, the quality is generally considered comparable to that sold in the U.S. Both countries have rigorous regulatory bodies that follow similar standards to ensure pharmaceutical products are safe and effective.
Regulatory Oversight
- Health Canada: This is Canada’s federal regulator, similar to the U.S. Food and Drug Administration (FDA). It is responsible for assessing and monitoring the safety, efficacy, and quality of drugs sold in Canada.
- Approval Process: Both Health Canada and the FDA require substantial scientific evidence from manufacturers before a drug can be authorized for sale.
- Manufacturing Standards: Canadian-licensed manufacturers and distributors must comply with Good Manufacturing Practices (GMP) and are subject to regular inspections. Canada is also a member of the Pharmaceutical Inspection Co-operation Scheme (PIC/S), an international effort to harmonize inspection standards across member countries.
Brand-name vs. generic drugs
- Brand-name drugs: Many brand-name drugs sold in Canada are produced by the same global manufacturers in the same factories as those sold in the U.S., and are often identical products.
- Generic drugs: Generic drugs in Canada, like those in the U.S., are required to be bioequivalent to their brand-name counterparts. This means they contain the same active ingredients and are designed to work the same way in the body. Any difference in appearance or inactive ingredients is not a quality issue and is typical for generics.
What Is the Ordering Process Like at an Online Canadian Pharmacy?
Shopping for prescription medications through reputable Canadian online pharmacies should be straightforward and user-friendly. The process mirrors what you’d expect from any trusted e-commerce platform: browse available medications, complete your purchase securely, and receive timely delivery to your doorstep.
MedicationsCanada.com prioritizes making your prescription ordering experience as smooth as possible through comprehensive behind-the-scenes support.
Our licensed pharmacy team meticulously reviews every prescription to ensure proper dosing and drug interactions, while our responsive customer support staff stands ready to assist with inquiries and can facilitate telephone orders when preferred. To get started, you’ll simply need three essential items: a current prescription from your healthcare provider, your shipping details, and your payment method of choice.
FAQs
Can U.S. doctors send prescriptions to Canada?
The ability for U.S. doctors to send prescriptions to Canada varies depending on the specific procedures and policies of the online Canadian pharmacy in question. Most Canadian online pharmacies accept prescriptions sent directly from American physicians through secure electronic transmission or fax. When direct submission isn’t supported, your healthcare provider can simply provide you with a physical prescription that you can then submit to your chosen Canadian pharmacy through their online portal or mail service.
Do Canadian pharmacies accept U.S. insurance?
Unfortunately, Medications Canada cannot process U.S. insurance plans directly. The logistical and regulatory complexities involved in working with American insurance providers make it impractical for Canadian online pharmacies to accept these plans. However, this limitation often works in your favor. By operating independently of insurance networks, we eliminate the extensive administrative processes and paperwork typically required for insurance claims. This streamlined approach allows us to reduce operational costs and pass those savings directly to our customers.
Additionally, many patients discover that their insurance coverage isn’t as reliable or comprehensive as they initially expected. It’s not uncommon for Americans to find that their insurance doesn’t cover certain medications or to experience unexpected coverage changes when insurers modify their formularies without notice. Establishing a dependable source for your medications through our pharmacy can provide greater consistency and peace of mind for your long-term healthcare needs. As an added benefit, we’re happy to provide detailed receipts that you can submit to your insurance company for potential reimbursement. In many cases, our cash prices are actually lower than the co-payments you’d pay at U.S. pharmacies for the same medications.
How do I get a prescription filled in Canada?
As an American resident, you can get your prescriptions filled online by a Canadian pharmacy through MedicationsCanada.com. We understand that ordering internationally requires some guidance, and so we answered frequently asked questions, which you can access by clicking here. You can also call us toll-free at +1-866-481-5817.
Do you need a prescription for a Canadian pharmacy?
Yes, all legitimate Canadian pharmacies require prescriptions. Any pharmacy claiming to sell prescription drugs without requiring prescriptions may be deemed unsafe.
How do refills work? Can I get a prescription refilled in Canada?
Yes, you can get a prescription refilled in Canada. Canadian pharmacies can fulfill a refill request as long as you provide a prescription written by a doctor to refill medications.
Conclusion
Getting your U.S. prescriptions filled through legitimate Canadian pharmacies offers a proven pathway to significant medication savings without compromising safety or quality. Through the secondary medical review process, proper regulatory oversight from Health Canada, and organizations like CIPA that vet pharmacy credentials, you can access the same high-quality medications at a fraction of U.S. prices.
The key to success lies in doing your homework: verify CIPA certification, confirm proper licensing, ensure prescription requirements are met, and choose pharmacies that provide clear contact information and customer support. While the process may seem unfamiliar initially, reputable Canadian online pharmacies like MedicationsCanada.com have streamlined the experience to be as simple as any trusted e-commerce purchase.
References
- National Library of Medicine. (2021). Determining the prevalence and risk factors for prescription drug unaffordability
- ASPE.hhs.gov. (2024). Comparing Prescription Drugs in the U.S. and Other Countries: Prices and Availability
- National Library of Medicine. (2024). International Prescription Drug Price Comparisons: Estimates Using 2022 Data
- CIPA.com. (2025). Licensed, Certified, Trusted
- CIPA.com. (2025). Buying Safe Online Prescription Drugs from Canada
- CIPA.com. (2025). CIPA Certification Mark
- National Library of Medicine. (2021). Evaluation of pharmacists’ awareness of illegal online pharmacies and perceived impact on safe access to medicines
- Health Canada. (2021). Choosing a safe online pharmacy
- Health Canada. (2012). Buying drugs online
- NAPRA.ca. (2025). Online Pharmacies
- National Library of Medicine. (2023). Quality and quantity of data used by Health Canada in approving new drugs
- Health Canada. (2024). Guidance document: Labelling of pharmaceutical drugs for human use
- Health Canada. (2019). Draft Guidance Document: Generic Drug Equivalence: Medicinal Ingredients
- Health Canada. (2016). About drug inspections
- KFF.org. (2024). FAQs on Prescription Drug Importation
- National Library of Medicine. (2023). Provincial experiments aim to lower public drug plan costs
- Health Canada. (2025). Review Process
- National Library of Medicine. (2013). The road to competitive generic drug prices in Canada
- Health Canada. (2025). Generic Drug Pricing and Access in Canada: What are the implications?
- National Library of Medicine. (2002). No direct-to-consumer drug ads: CMA
- National Library of Medicine. (2015). Delays in the submission of new drugs in Canada
- Health Canada. (2025). Drugs and health products
- Health Canada. (2020). Community Pharmacy Inspection Program Annual Report, Fiscal Year 2019–2020
- ABPharmacy.ca. (2025). Standards for the Operation of Licensed Pharmacies
- NAPRA.ca. (2019). CS-GD-022 – Recommended guidance in the areas of security, inventory reconciliation and record-keeping for community pharmacists
- PEBC.ca. (n.d.). General Information
- NAPRA.ca. (2022). Model Standards of Practice for Pharmacists and Pharmacy Technicians in Canada
- FDA.gov. (2025). Counterfeit Medicine
- Health Canada. (2021). Choosing a safe online pharmacy
- FDA.gov. (2021). FDA’s Decade-Long Participation in the U.S.-Canada Regulatory Cooperation Council
- National Institutes of Health. (2013). An Overview of Canadian and U.S. Approaches to Drug Regulation
- Health Canada. (2024). Access to Generic Drugs in Canada
- U.S. Government Publishing Office. (2016). Prescription Drug Reimportation
- Health Canada. (2020). Guidelines for Temperature Control of Drug Products during Storage and Transportation (GUI-0069)
- Health Canada. (2020). Guidance on Drug Establishment Licences (GUI-0002)
- National Association of Boards of Pharmacy. (2020). Addressing Prescription Drug Importation and Patient Safety
- Health Canada. (2020). Frequently Asked Questions: Subsection 56(1) Class Exemption for Patients, Practitioners, and Pharmacists Prescribing and Providing Controlled Substances in Canada
Why Is Eliquis So Expensive (And How to Get It for About $1 Per Pill)

If you’ve ever been prescribed Eliquis, you may have experienced sticker shock at the pharmacy counter. As one of the most widely used blood thinners, Eliquis plays a crucial role in preventing strokes and blood clots. But its price can be staggering. Without insurance, a one-month supply can cost between $400 and $600, making it a financial burden for many Americans seeking care. But why is Eliquis so expensive? From patent protections and research costs to the lack of pricing regulations in the U.S., several factors contribute to its high price tag. In this article, we’ll break down the reasons behind the high cost of Eliquis and explore how you can save money on this essential medication.
What is Eliquis?
Eliquis, with the generic name apixaban, is an oral anticoagulant (blood thinner) that belongs to the drug class of Factor Xa inhibitors. It works by blocking Factor Xa, a protein necessary for blood clotting, thereby reducing the formation of clots in the blood.
What is Eliquis Used for?
Eliquis is used to reduce the risk of stroke and blood clots in people who have atrial fibrillation. It reduces the risk of forming a blood clot in the legs and lungs of people who have just had hip or knee replacement surgery. Eliquis treats blood clots in the veins of your legs (deep vein thrombosis) or lungs (pulmonary embolism), and reduces the risk of them occurring again.
How Much Does Eliquis Cost?
Without insurance, Eliquis may cost between $400 – $600 for a 30-day supply, depending on dosage and pharmacy location. Medicare and insurance plans may reduce costs significantly, but out-of-pocket expenses vary based on the coverage.
Is Eliquis The Most Expensive Blood Thinner?
Eliquis is among the most expensive blood thinners on the market, but it is not the absolute costliest. Blood thinners, also known as anticoagulants, are essential medications for preventing strokes, blood clots, and other cardiovascular complications. However, their pricing varies significantly depending on the brand, availability of generics, and insurance coverage.
As of 2024, the average retail price for a 30-day supply of Eliquis (5 mg, 60 tablets) in the U.S. is around $642, translating to about $10.70 per tablet. For a 168-tablet supply, the cost exceeds $1,765.52. This makes Eliquis one of the priciest options, particularly for those without insurance. Compared to older blood thinners like warfarin, which cost as little as $10 to $30 per month, the difference is staggering.
However, Eliquis is not the most expensive anticoagulant. Pradaxa (dabigatran), another direct oral anticoagulant (DOAC), can cost over $550 for a 30-day supply, while Xarelto (rivaroxaban) is priced at around $600 per month. The high cost of these medications is largely due to patent protections, research and development expenses, and the lack of widely available generics in the U.S.
Patients looking for more affordable alternatives often consider international pharmacies, where the same medications can be significantly cheaper. For example, in Canada, a 168-tablet supply of brand-name Eliquis costs around $174, nearly 90% less than in the U.S. Generic versions (apixaban) are also available in Canada and other countries at a fraction of the price. While Eliquis is undoubtedly expensive, it remains one of the most effective and widely prescribed blood thinners due to its lower risk of bleeding complications compared to warfarin. The high cost, however, continues to be a major concern for patients seeking affordable long-term treatment.
Why is the price of Eliquis so high?
The high price of Eliquis is due to several factors:
Patent protection
Eliquis has been a subject of discussion due to its high cost in the United States. One of the primary reasons for its expensive price tag is patent protection, a crucial factor in the pharmaceutical industry. Patent protection grants pharmaceutical companies exclusive rights to produce and sell their newly developed drugs for a specific period, typically around 20 years. This exclusivity allows pharmaceutical companies to recoup their substantial investments in research and development. In the case of Eliquis, Bristol Myers Squibb and Pfizer, the drug’s manufacturers, have managed to extend their patent protection through various legal means.
Although the U.S. Food and Drug Administration approved generic versions of Eliquis (apixaban) in 2020, the brand-name medication has maintained its patent exclusivity in the U.S. market. Thanks to successful legal challenges and settlements, Bristol Myers Squibb and Pfizer have fended off cheaper alternatives until at least 2026, with some sources indicating that generics may not enter the market until April 2028. This extended period of exclusivity has significant implications for consumers. Without generic competition, Eliquis can command a premium price in the U.S. market, often costing over $500 for a month’s supply. The lack of alternatives leaves patients and healthcare systems with limited options, contributing to the ongoing debate about prescription drug pricing in America.
Research and development costs
Developing innovative drugs involves significant investment. Research and development (R&D) costs play a significant role in the high price of Eliquis. Pharmaceutical companies often cite these expenses as a key factor in setting drug prices. The process of developing a new drug is lengthy and costly. On average, it takes 12-13 years and approximately $1.4 billion to bring a new medication to market. This substantial investment covers various stages of drug development, including early discovery, preclinical testing, and multiple phases of clinical trials.
For Eliquis specifically, while exact figures aren’t publicly available, it’s reasonable to assume that its development followed a similar pattern of high investment. However, it’s important to note that the relationship between R&D costs and drug pricing is complex.
While pharmaceutical companies argue that high prices are necessary to recoup their investments, critics point out that many top-selling drugs, including Eliquis, have generated revenues far exceeding their development costs. For instance, Medicare alone spent $27.2 billion on Eliquis between 2016 and 2020, which is more than ten times the average cost to develop a new drug.
Furthermore, research has shown that many pharmaceutical companies spend more on stock buybacks and dividends than on R&D. This suggests that while R&D costs are a factor in drug pricing, they are not the sole determinant.
As research continues and pricing practices evolve, the debate over the true impact of R&D costs on drug prices is likely to persist.
Lack of pricing regulations
The U.S. does not cap drug prices, allowing manufacturers to set high rates.
One of the key factors contributing to the high cost of Eliquis in the United States is the lack of pricing regulations for prescription drugs. Unlike many other developed countries, the U.S. government does not impose restrictions on how much pharmaceutical companies can charge for brand-name medications. This absence of price controls allows drug manufacturers to set prices based on what the market will bear, rather than on factors such as production costs or affordability for patients. As a result, the same medication can cost significantly more in the U.S. compared to other countries.
The stark price difference is further exacerbated by the inability of government programs like Medicare to negotiate drug prices directly with pharmaceutical companies. This limitation, coupled with extended patent protections, enables manufacturers to maintain high prices for brand-name drugs like Eliquis without facing significant market pressures to reduce costs.
The impact of this lack of pricing regulation is profound, with many American customers struggling to afford their necessary medications. While some relief may be on the horizon, with Medicare beginning to negotiate prices for certain drugs, the current system continues to place a significant financial burden on patients and the healthcare system as a whole.
Customers without insurance – Impact?
Although generic versions of Eliquis were FDA-approved in 2020, legal disputes have delayed their availability. Current patents extend exclusivity until November 2026, meaning generics likely won’t be widely available until after this date.
The high cost of Eliquis has a significant impact on uninsured patients in the USA:
- Financial burden: Uninsured consumers typically pay a lot more for a 30-day supply of Eliquis, depending on dosage and quantity. This high price can make it extremely difficult for patients to afford their prescribed treatment.
- Full price payment: Uninsured consumers, with no one to negotiate on their behalf, are forced to pay full price for their medications—if they are able to afford them at all.
- Limited access: The high cost may lead some uninsured consumers to ration their medication or forgo treatment entirely, potentially compromising their health outcomes.
The Cheapest Way to Get Eliquis
How to Pay About $1 Per Pill?
Many Americans facing high prescription drug costs have found relief through international and Canadian online pharmacies, which offer significantly lower prices on essential medications. This practice has deep roots, dating back to the early 2000s when an Ohio state senator organized bus trips across the Canadian border to help seniors access affordable prescriptions.
This trend continues today. In 2019, CBC News documented a renewed surge in Americans seeking medications north of the border. The report revealed that some physicians now directly contact Canadian pharmacies to arrange prescriptions for their patients, while those living near the Canadian border simply make the drive themselves. The convenience factor makes this option even more attractive. Rather than traveling internationally, Americans can now order their prescriptions online from home and have them delivered directly to their doorstep, combining substantial cost savings with the ease of home delivery.
You can access a Canadian pharmacy through MedicationsCanada.com to buy a 56-tablet supply of Eliquis for $63.95. Navigating prescription drug costs is always stressful and overwhelming. Our goal is to help you save money. To save money on your prescription medications, call us toll-free at +1-866-481-5817.
Opt for 90-Day Supplies
Purchasing a 90-day supply of Eliquis can further reduce costs:
- Lower per-pill cost: Buying in bulk often results in a lower price per tablet.
- Fewer pharmacy trips: This means fewer copays if you have insurance.
- Convenience: You’ll need to refill your prescription less frequently.
At MedicationsCanada.com, a 168-tablet supply (approximately 90 days) of Eliquis 5mg is priced at $173.95, offering even greater savings compared to smaller quantities.
By combining these two strategies, purchasing from a Canadian pharmacy and opting for a 90-day supply, you can significantly reduce your Eliquis expenses while ensuring a consistent supply of this crucial medication.
References
- Eliquis Prescribing Information. 2012. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/202155s012lbl.pdf
- Eliquis Prices, Coupons, Copay Cards & Patient Assistance. 2025. https://www.drugs.com/price-guide/eliquis
- Pradaxa Prices, Coupons, Copay Cards & Patient Assistance. 2025. https://www.drugs.com/price-guide/pradaxa
- Xarelto Prices, Coupons, Copay Cards & Patient Assistance. 2025. https://www.drugs.com/price-guide/xarelto
- Top 10 drugs with patents due to expire in the next five years. 2024. https://www.proclinical.com/blogs/2024-2/top-10-drugs-with-patents-due-to-expire-in-the-next-5-years
- Investor Statement on Eliquis Revenue Under IRA. 2024. https://www.bms.com/investor-statement-on-eliquis-revenue-under-ira.html
- Pharmaceutical industry profile. 2024. https://ised-isde.canada.ca/site/canadian-life-science-industries/en/biopharmaceuticals-and-pharmaceuticals/pharmaceutical-industry-profile
- Medicare Spending on Prescription Drugs Far Outpaces Development Costs. 2022. https://www.aarp.org/politics-society/advocacy/info-2022/medicare-prescription-drug-spending.html
- Medicare now negotiating price of drug that costs $7,100 in US vs. $900 in Canada. 2024. https://www.cnn.com/2024/02/06/politics/medicare-drug-prices-eliquis-bernie-sanders/index.html
- 6 Savings Tips for Eliquis While Its Generics Are on Hold. 2020. https://www.goodrx.com/eliquis/eliquis-generics-approved-patent-expiration-ways-to-save
- Paying the Price. 2006. https://pirg.org/wp-content/uploads/2012/01/PayingthePriceDC_0.pdf
- Eliquis and Cost: What You Need to Know. 2023. https://www.healthline.com/health/drugs/eliquis-cost#next-steps
What is COPD
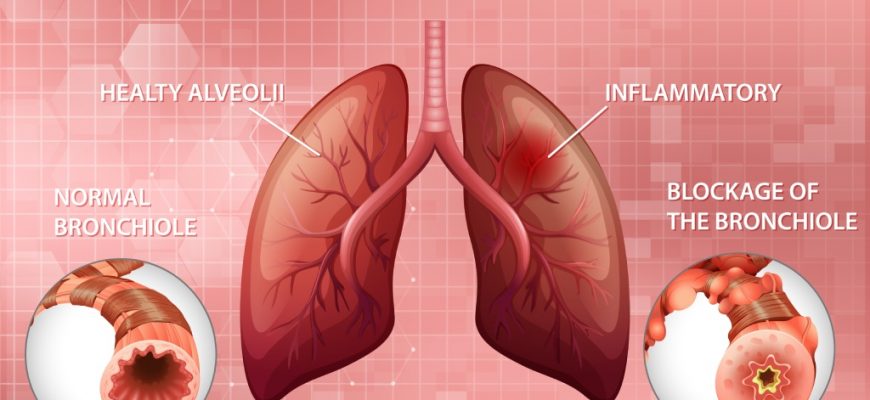
What is COPD?
COPD, also known as chronic obstructive pulmonary disease, is a long-term lung problem. It encompasses a variety of illnesses that impair breathing and impede airways. The most common progressive lung conditions are emphysema and chronic bronchitis.
Emphysema causes damage to the lungs’ air sacs, causing them to become less elastic. This damage results in the lungs being less effective at exchanging oxygen and carbon dioxide.
In chronic bronchitis, airway linings inflame. This causes too much mucus. Once bronchitis becomes persistent and unresponsive to treatment, it becomes chronic.
Our COPD data comes from short studies. These studies tracked patients for 5-10 years. COPD, in reality, develops over many decades. This development is a slow process.
Emphysema causes damage to the lungs’ air sacs, causing them to become less elastic. This damage results in the lungs being less effective at exchanging oxygen and carbon dioxide.
How does COPD affect your lungs?
With COPD, the lungs’ small air sacs and airways lose the ability to expand and contract because of damage. The airway walls become inflamed, produce mucus, and restrict airflow. Untreated COPD worsens, leading to heart problems and frequent infections. Note that this condition is not contagious, and there are several factors that can trigger it.
What causes COPD?
Most people who are at high risk of having COPD conditions are as follows:
- Middle-aged adults (40 years old or older) with a history of tobacco smoking
- Prolonged exposure to heavy amounts of secondhand smoke
- Exposure to toxins (fumes or chemicals) at home or in the workplace
- Long-term exposure to air pollution
- Genetic factor (a rare condition in which there is a lack of alpha-1 antitrypsin protein)
- Usage of a cooking fire regularly without enough ventilation
- Family history of COPD
- History of severe asthma
COPD Symptoms
Breathing becomes more difficult with COPD. Signs include breathlessness, persistent cough, and thick mucus production. As it worsens, symptoms become more frequent, making breathing increasingly difficult. Symptoms vary depending on COPD stages.
Stage I: Initial Symptoms
- Periodically having breathing problems, especially after exercising
- A mild yet persistent cough (productive or dry cough)
- Frequently needing to clear your throat, especially in the early morning
Stage II: Moderate Symptoms
- Shortness of breath after exertion
- Difficulty sleeping
- Wheezing during exhalations
- Chronic persistent cough with or without mucus
- Lack of energy
Stage III: Severe Symptoms
- Coughing and shortness of breath have increased in intensity
- A lot of flare-ups
- Lung infections (recurrent colds, bronchitis, or pneumonia)
- Chest tightness
- Wheezing when doing daily tasks
- Legs, ankles, or feet swelling
Stage IV: Very Severe Symptoms
- Stage 3 symptoms become more severe
- Shortness of breath is present, even when a person is resting
- Weight loss
- Delirium
- Barrel chest
- Increased heart rate
- Hypertension in the pulmonary artery
COPD Diagnosis
There isn’t a single test for this lung problem. Symptoms, a physical examination, medical history, and the findings from diagnostic tests all contribute to the diagnosis. Tests may include:
- Chest exam to assess breathing with a stethoscope
- Chest X-ray to look for problems in the lungs
- CT scan detailed scan to identify lung problems
- Spirometry to assess lung function
- Arterial blood test to check the oxygen levels in the blood
- Diffusing capacity (DLCO) to measure how well your lungs exchange oxygen and carbon dioxide
Other tests may include confirming and determining the severity of chronic obstructive pulmonary disease:
- Electrocardiogram (ECG)is to identify whether a heart disease rather than a lung problem is the source of the shortness of breath.
- Peak flow test, the score measures how quickly you can exhale and can tell you if your airways are congested.
- Sputum tests determine the cause of your breathing difficulties.
- Pulmonary function tests check your ability to breathe in and out and see if your lungs are supplying your blood with enough oxygen.
4 Stages of COPD
COPD has four stages based on GOLD guidelines for care. GOLD groups COPD from Grade 1 to 4 and Group A to D. This helps doctors check how blocked your airways are using a breathing test.
A spirometer measures forced vital capacity (FVC), the total amount of air you can exhale at once. Also, it will help assess forced expiratory volume in 1 second (FEV1), the amount of air you can forcefully release in the first second.
- GOLD COPD Grade 1 Mild FEV1 is 80% or higher
- GOLD COPD Grade 2 Moderate FEV1 is between 50% and 79%
- GOLD COPD Grade 3 Severe FEV1 is between 30% and 49%
- GOLD COPD Grade 4 Very severe FEV1 is less than 30%
Note that the diagnosis of COPD patients is confirmed if the FEV1/FVC is less than 70%.
COPD treatment
COPD cannot be cured, but you can manage it to feel better and stay out of the hospital. You can take steps to reduce symptoms and slow the disease. The best way to do this is to quit smoking. Stay away from smoke and dirty air that can hurt your lungs. Simple lifestyle changes can help you breathe easier and avoid serious problems. Your doctor may also suggest medicines and other treatments.
- Medicines that quickly open the airways, reduce inflammation and swelling, and treat infection
- Supplemental oxygen if needed
- Pulmonary rehabilitation treatment program (breathing exercises, conserving energy, and eating habits)
- Vaccines to prevent lung infection
- Surgery (if conditions become severe and other treatments do not work)
What is COPD exacerbation?
COPD flare-ups happen when breathing problems get worse. They can last for days or weeks and may need medicine or a hospital stay. In later stages, flare-ups happen more often as the lungs get weaker. Each flare-up can cause lasting lung damage. They are usually caused by lung infections but can also be triggered by smoking, smoke, or air pollution. Make sure to watch out for symptoms of exacerbation including:
- Frequent coughing, wheezing, or breathing difficulties than usual
- Mucus changes (color, thickness, or quantity)
- Fatigue that lasts for more than one day
- Swelling in legs or ankles
- Trouble sleeping
- Being on oxygen and trouble catching your breath
Patients can also lower the risk of exacerbation by doing the following:
- Following the treatment plan
- Take your medicine regularly
- Automate prescription refills
- Keep loved ones and friends informed
- Avoiding triggers
- Avoid tobacco smoke
- Quit smoking
- Household dust
- Pollution
- Getting vaccinated
- Flu or pneumonia vaccine
COPD Medications
COPD medicines help control symptoms and prevent serious health problems. Treatment eases symptoms, lowers risks, and slows the disease.
Your doctor may prescribe you to use:
- Short-acting bronchodilators (e.g., Albuterol): Bronchodilators open and loosen tight airways as quickly as possible when breathing becomes more difficult than usual. They can ease respiratory symptoms such as coughing and shortness of breath for four to six hours.
- Long-acting bronchodilators (e.g., Salmeterol): It helps keep airways relaxed for up to 12 hours. Regular use may lessen COPD flare-ups and assist in enhancing lung function.
- Corticosteroids (e.g. Budesonide): Steroid inhalers aid in decreasing the inflammation of the airways. They can also help reduce exacerbation.
- Antibiotics: Antibiotics kill the bacteria causing the infection (e.g., pneumonia) to prevent the worsening of COPD symptoms. Patients with COPD are more likely to develop more severe pneumonia, increased hospital admissions, and worse outcomes.
Apart from this regimen, Trelegy Ellipta is an inhaler used as a maintenance treatment for patients with moderate to severe COPD.
COPD makes daily tasks harder by causing breathing problems, mucus, wheezing, and chest tightness.
It is important to let your healthcare provider know if you experience these symptoms and stop smoking. Proper COPD care can enhance your functional abilities, exercise tolerance, and improve your quality of life, preventing potentially fatal complications associated with COPD.
References
Basics About COPD. 2023
COPD Causes and Risk Factors. 2024.
Four stages of COPD. 2024.
Overactive Bladder (OAB): Causes, Diagnosis, Symptoms, Treatment

Overactive bladder (OAB) results in frequent, unexpected bathroom urges that can be challenging to control. You can experience frequent urges to pee during the day and at night, as well as involuntary urination (urgency incontinence).
OAB is also called “spastic bladder” or “irritable bladder” that affects many individuals across the globe.
It can be physically and emotionally taxing to have a bladder condition, affecting your daily activities. It can be annoying; at worst, it can be crippling. when urine incontinence is involved, it can also lead to anxiety, embarrassment, and even despair.
OAB may also have an impact on your relationships with your friends and family. In addition, your sleeping pattern may be disturbed due to frequent urination,. Moreover, if there is a leak of urine, you could be more prone to infections, like urinary tract infections (UTIs).
What causes overactive bladder (OAB)
The signals involved in emptying a bladder are complex. Normally, urine from the kidneys flows into the bladder. The sphincter muscle functions as a faucet and regulates urine flow while the bladder expands to hold the urine. As the bladder fills, nerve signals are sent to the brain that prompts the urge to urinate. The brain sends the signal to the bladder to hold on until a person consciously decides to go. Urine is emptied out of the bladder through conscious contraction of the bladder muscle.
With OAB, nerve signals between the brain, spinal cord, and bladder are not functioning well. There may be abnormalities with the urethra, bladder, or urinary sphincter. The bladder may contract without voluntary control, or the urethral sphincter may not be closing properly or resisting the flow of urine from the bladder, leading to leakage.
Possible causes of overactive bladder include:
- Brain or spinal cord problems (e.g., stroke or multiple sclerosis)
- Diabetes mellitus
- Urinary tract infections (UTI)
- Bladder tumors, polyps, or stones
- Hormone changes in women going through menopause
- Drinking excessive amounts of caffeine or alcohol
- Side effects of certain medications (e.g., water pills)
- Decreased cognitive functioning due to aging
- Inadequate emptying of the bladder
What are the symptoms of overactive bladder (OAB)
The overactive bladder symptoms are as follows:
- You have the sudden desire to urinate that is hard to control
- Involuntary loss of urine right after an urgent need to urinate (urgency incontinence)
- Urinating more often, typically eight or more times in 24 hours
- Getting up in the middle of the night during sleeping hours more than two times to urinate (nocturia)
How do you diagnose an overactive bladder (OAB)
When you have consulted your symptoms with your healthcare provider, they will typically do an assessment immediately. They could also suggest a specialist, like a urologist, who specializes in diagnosing and treating patients with OAB.
Most of the time, OAB can be confirmed with the following to rule out any underlying conditions:
- Medical history
- Physical examination (e.g., rectal exam and pelvic exam)
- Urine study to screen for an infection, blood traces, or other problems
- Comprehensive neurological assessment that may detect sensory or reflex problems
Additional testing may be performed in more complicated cases. These tests will help healthcare providers gain more knowledge of the lower urinary tract’s structure and function. These tests could consist of the following:
- Urodynamic tests evaluate how well your bladder is working and whether it can consistently empty fully.
- Ultrasound (bladder scan) to assess how much urine is left in your bladder after you urinate or if the bladder is emptying well
- Uroflowmeter to monitor voiding volume and rate
- Cystometry to check how well the bladder is functioning. It is indicated to check for problems with the filling and emptying of the bladder. Also, it is used to identify if you have uncontrollable muscular spasms or a rigid bladder that cannot hold urine under low pressure.
How to treat overactive bladder (OAB)
Once you have been diagnosed with OAB, patients can explore potential treatments with their doctor. Discussing will aid in your understanding of the root of your issue and the possible benefits of various therapies. In addition, your doctor will discuss any potential side effects associated with a given course of treatment.
The following are the overactive bladder treatments or strategies:
Behavioral Therapies are the most effective method for controlling OAB and have no harmful side effects.
- Pelvic floor muscle rehabilitation (Kegel’s exercise) helps strengthen the pelvic floor muscles and urinary sphincter, preventing the involuntary contractions of the bladder.
- Biofeedback, a mechanism in which sensors are attached to your body to help you receive information about your body and make subtle changes
- Weight loss
- Schedule urination, which helps you develop a regular routine to urinate, and does not rely on the urge
- Intermittent catheterization, in which a device is inserted in the urethra to help you empty your bladder if the bladder cannot do so by itself
- Absorbent pads, which helps protect you and your clothing from leakage
- Bladder training, which helps you hold in the urine until you are ready
Medications
Numerous pharmacological therapies are effective in treating OAB. Your doctors can provide you with advice on what medications might be best for you depending on your symptoms, your other medical problems, the prescriptions you are currently taking, and the adverse effect profile of medicines.
- Vaginal estrogen therapy to help strengthen the muscles and tissues in the urethra and vaginal area
The symptoms of an overactive bladder can sometimes be relieved by taking medications that relax the bladder like:
- Tolterodine (Detrol)
- Oxybutynin (Ditropan XL), (Oxytrol), or (Gelnique)
- Trospium
- Solifenacin (Vesicare)
- Fesoterodine (Toviaz)
- Mirabegron (Myrbetriq)
- Bladder injections
- OnabotulinumtoxinA helps relax the muscles
Nerve stimulation
The symptoms of OAB can be improved by controlling the nerve impulses to your bladder.
- Percutaneous tibial nerve stimulation (PTNS)
This procedure transmits electrical impulses from the tibial nerve to your spine, where it connects to control the bladder.
Surgery
Surgery is only used to treat OAB in cases where the symptoms are severe and other treatments are ineffective. The intention is to lessen bladder pressure and increase the capacity of the bladder to hold urine.
- Bladder removal
Conclusion
Overactive bladder is characterized by a sudden, intense urge to urinate that is challenging to put off, including frequent urination, nocturia, and urinary incontinence.
With OAB, some individuals can have a profound effect on their quality of life. OAB disrupts the ability to accomplish daily tasks and curtails social functions such as work, travel, physical activity, sleep, and sexual function.
However, it is essential to be aware that symptoms of OAB can be effectively treated. These treatments can range from behavioral therapies, medications, minimally invasive procedures, and surgery.
Although it may seem odd to discuss something so personal with your doctor about bladder problems, seeking medical assistance is the first stage of treatment to overcome this medical condition.
How Xifaxan Can Help Treat Diarrhea & Constipation?

Learn how prescription medication XIFAXAN can help treat irritable bowel syndrome with diarrhea (IBS-D), including abdominal pain and constipation.
There is nothing worse than a sudden upset stomach and an unwanted bout of diarrhea. Typically, these bouts pop up at the most inopportune times like travelers’ diarrhea and can cause severe discomfort in all of the wrong places.
On the other hand, suffering from the inability to produce a bowel movement on a regular basis (also known as constipation) can be equally as uncomfortable and painful.
If you suffer from diarrhea or constipation, your body is not working as it should it could be caused by bacterial overgrowth and may need assistance such as antibiotics. Diarrhea is characterized as loose or watery stools that usually occur when you’re sick or fighting an infection.
If you suffer from diarrhea frequently for more than 2–3 days at a time, you might need medical assistance to get your bowels under control.
Constipation is characterized as the inability to produce bowel movements on a regular basis. When bowel movements do occur, they might be hard or painful.
How to Know if You Have Diarrhea?
Sometimes our bowel movements have a mind of their own. This can create confusion when you don’t know quite what you’re dealing with, which can make treatment for relief more difficult.
If you are wondering if you are suffering from diarrhea, here are a few common symptoms you may be experiencing:
- Bloating in your abdomen
- Moderate to severe cramps
- Watery or loose stools
- A sudden need to use the restroom
- Nausea or vomiting (not frequent)
There are more severe and concerning symptoms that should be taken seriously if ever observed during a diarrhea bout:
- Fever
- Unexplained weight loss (not due to exercise or diet)
- Bloody stool
What Causes Diarrhea?
Every person responds differently to illness, infections, or other medical conditions. There are some common causes of diarrhea, though, that many diarrhea sufferers have reported:
- Virus
- Flu
- Certain medications
- Malabsorption (the inability to absorb needed nutrients)
- Alcoholism
- Food poisoning
- Adverse reactions to certain foods
- Allergies to certain foods
If you do suffer from diarrhea, you may be more susceptible to dehydration. This can be a dire condition if not treated properly. Some common warning signs of dehydration include dark urine, less frequent urination, and headaches.
Call your doctor immediately if you experience any of the less-than-common symptoms of diarrhea as well as signs of dehydration!
How to Know if You Have Constipation?
On the flip side of diarrhea is constipation. This is a condition that is characterized by the inability to produce bowel movements or painful stools. While this is not typically a worrisome problem to have, it can certainly be painful. When your body gets back on track and produces frequent bowel movements, everything will run much smoother.
If you are not sure whether or not you have constipation, here are some common symptoms that may arise:
- Painful stools
- Abdomen bloating
- Fewer bowel movements
- Difficulty while trying to produce a bowel movement
- Small, round pellet stools
What Causes Constipation?
There are some common reasons you might suffer from constipation. This condition is not usually a serious concern, but finding out the root cause of the issue can help you find the right treatment. Here are just some common causes of constipation:
- Pregnancy
- Lack of fiber in your diet
- Change to your diet or activity level
- Less-than active lifestyles
- Stress
- Irritable bowel syndrome (IBS)
- Underactive thyroid
Now that you are aware of whether or not you’re suffering from diarrhea or constipation, it is time to talk about solutions! Your body deserves to have regular, healthy bowel movements. Once you can alleviate whichever problem you are suffering from, you can start living a healthy and happy life once again!
How to Stop Diarrhea?
Inconvenience, uncomfortableness, and pain all describe diarrhea for most people. Here are some common ways to get rid of diarrhea quickly:
- The BRAT Diet
IBS and diarrhea are both extremely uncomfortable and highly inconvenient for anyone. If you suffer from a sudden onset of diarrhea or chronic IBS, you may want to incorporate the BRAT diet for a while into your daily life.
The BRAT diet consists of:
- Bananas
- Rice
- Applesauce
- Toast
This will not cure your diarrhea or IBS symptoms, but this combination is easier on your stomach and can provide relief from the constant working of your body to accommodate unique foods.
- Water! Water! Water!
Staying hydrated is the key to keeping infectious diarrhea from bacteria and IBS at bay. Both of these bowel movement issues can cause severe dehydration if you’re not careful; therefore, it is very important that you keep your body full of water at all times. The water can also give your body back the nourishment it needs to feel better quickly.
- Medication like Xifaxan
If changing your diet or waiting out a virus doesn’t do the trick, you may need to employ a more aggressive approach to get IBS or diarrhea to stop! Medications are great for helping sufferers alleviate their symptoms and find balance in their bodies once again.
XIFAXAN is a medication that was created specifically to stop IBS or acute diarrhea in the intestine and give your body back the normalcy it deserves. This medication works to prevent the three most common symptoms of IBS with diarrhea:
- Severe abdominal pain and cramps with diarrhea
- Diarrhea
XIFAXAN works as a 2-week treatment plan that can provide relief for up to six months for sufferers. This is one of the only medications that offer this type of treatment plan, and it has been proven to be highly effective in treating IBS with diarrhea.
If you are tired of suffering from IBS with diarrhea or diarrhea on its own, it’s time to pull out the big guns such as XIFAXAN! Talk to your doctor as soon as possible to find out if this medication is right for you.
How to Get Rid of Constipation?
Since constipation is not a cause for serious concern, there are some simple steps you can take to relieve your body of the painful and infrequent bowel movements:
- Stay hydrated as much as possible
- Add more fiber into your diet
- Keep moving and stay active
- Eat more fruits and vegetables
- Take stool softeners if needed
As you can see, diarrhea and constipation are unwanted visitors in many people’s lives. Finding the right solution for your body will make a world of difference and give you back the life you deserve.