What is COPD?
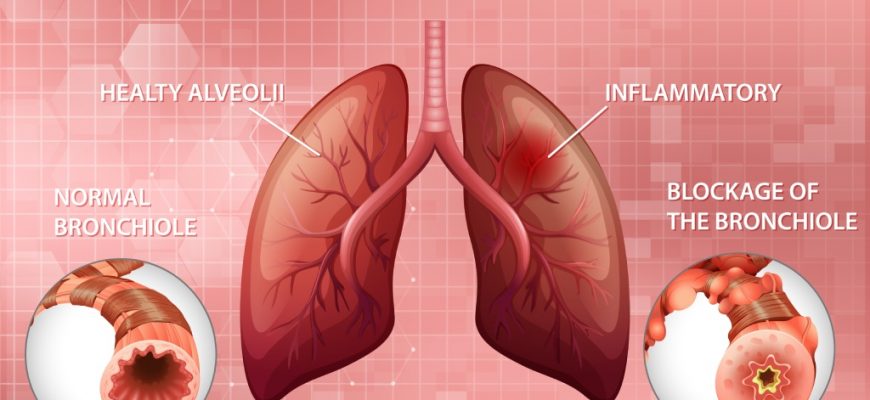
COPD, also known as chronic obstructive pulmonary disease, is a long-term lung problem. It encompasses a variety of illnesses that impair breathing and impede airways. The most common progressive lung conditions are emphysema and chronic bronchitis.
Emphysema causes damage to the lungs’ air sacs, causing them to become less elastic. This damage results in the lungs being less effective at exchanging oxygen and carbon dioxide.
In chronic bronchitis, airway linings inflame. This causes too much mucus. Once bronchitis becomes persistent and unresponsive to treatment, it becomes chronic.
Our COPD data comes from short studies. These studies tracked patients for 5-10 years. COPD, in reality, develops over many decades. This development is a slow process.
Emphysema causes damage to the lungs’ air sacs, causing them to become less elastic. This damage results in the lungs being less effective at exchanging oxygen and carbon dioxide.
How does COPD affect your lungs?
With COPD, the lungs’ small air sacs and airways lose the ability to expand and contract because of damage. The airway walls become inflamed, produce mucus, and restrict airflow. Untreated COPD worsens, leading to heart problems and frequent infections. Note that this condition is not contagious, and there are several factors that can trigger it.
What causes COPD?
Most people who are at high risk of having COPD conditions are as follows:
- Middle-aged adults (40 years old or older) with a history of tobacco smoking
- Prolonged exposure to heavy amounts of secondhand smoke
- Exposure to toxins (fumes or chemicals) at home or in the workplace
- Long-term exposure to air pollution
- Genetic factor (a rare condition in which there is a lack of alpha-1 antitrypsin protein)
- Usage of a cooking fire regularly without enough ventilation
- Family history of COPD
- History of severe asthma
COPD Symptoms
Breathing becomes more difficult with COPD. Signs include breathlessness, persistent cough, and thick mucus production. As it worsens, symptoms become more frequent, making breathing increasingly difficult. Symptoms vary depending on COPD stages.
Stage I: Initial Symptoms
- Periodically having breathing problems, especially after exercising
- A mild yet persistent cough (productive or dry cough)
- Frequently needing to clear your throat, especially in the early morning
Stage II: Moderate Symptoms
- Shortness of breath after exertion
- Difficulty sleeping
- Wheezing during exhalations
- Chronic persistent cough with or without mucus
- Lack of energy
Stage III: Severe Symptoms
- Coughing and shortness of breath have increased in intensity
- A lot of flare-ups
- Lung infections (recurrent colds, bronchitis, or pneumonia)
- Chest tightness
- Wheezing when doing daily tasks
- Legs, ankles, or feet swelling
Stage IV: Very Severe Symptoms
- Stage 3 symptoms become more severe
- Shortness of breath is present, even when a person is resting
- Weight loss
- Delirium
- Barrel chest
- Increased heart rate
- Hypertension in the pulmonary artery
COPD Diagnosis
There isn’t a single test for this lung problem. Symptoms, a physical examination, medical history, and the findings from diagnostic tests all contribute to the diagnosis. Tests may include:
- Chest exam to assess breathing with a stethoscope
- Chest X-ray to look for problems in the lungs
- CT scan detailed scan to identify lung problems
- Spirometry to assess lung function
- Arterial blood test to check the oxygen levels in the blood
- Diffusing capacity (DLCO) to measure how well your lungs exchange oxygen and carbon dioxide
Other tests may include confirming and determining the severity of chronic obstructive pulmonary disease:
- Electrocardiogram (ECG)is to identify whether a heart disease rather than a lung problem is the source of the shortness of breath.
- Peak flow test, the score measures how quickly you can exhale and can tell you if your airways are congested.
- Sputum tests determine the cause of your breathing difficulties.
- Pulmonary function tests check your ability to breathe in and out and see if your lungs are supplying your blood with enough oxygen.
4 Stages of COPD
COPD has four stages based on GOLD guidelines for care. GOLD groups COPD from Grade 1 to 4 and Group A to D. This helps doctors check how blocked your airways are using a breathing test.
A spirometer measures forced vital capacity (FVC), the total amount of air you can exhale at once. Also, it will help assess forced expiratory volume in 1 second (FEV1), the amount of air you can forcefully release in the first second.
- GOLD COPD Grade 1 Mild FEV1 is 80% or higher
- GOLD COPD Grade 2 Moderate FEV1 is between 50% and 79%
- GOLD COPD Grade 3 Severe FEV1 is between 30% and 49%
- GOLD COPD Grade 4 Very severe FEV1 is less than 30%
Note that the diagnosis of COPD patients is confirmed if the FEV1/FVC is less than 70%.
COPD treatment
COPD cannot be cured, but you can manage it to feel better and stay out of the hospital. You can take steps to reduce symptoms and slow the disease. The best way to do this is to quit smoking. Stay away from smoke and dirty air that can hurt your lungs. Simple lifestyle changes can help you breathe easier and avoid serious problems. Your doctor may also suggest medicines and other treatments.
- Medicines that quickly open the airways, reduce inflammation and swelling, and treat infection
- Supplemental oxygen if needed
- Pulmonary rehabilitation treatment program (breathing exercises, conserving energy, and eating habits)
- Vaccines to prevent lung infection
- Surgery (if conditions become severe and other treatments do not work)
What is COPD exacerbation?
COPD flare-ups happen when breathing problems get worse. They can last for days or weeks and may need medicine or a hospital stay. In later stages, flare-ups happen more often as the lungs get weaker. Each flare-up can cause lasting lung damage. They are usually caused by lung infections but can also be triggered by smoking, smoke, or air pollution. Make sure to watch out for symptoms of exacerbation including:
- Frequent coughing, wheezing, or breathing difficulties than usual
- Mucus changes (color, thickness, or quantity)
- Fatigue that lasts for more than one day
- Swelling in legs or ankles
- Trouble sleeping
- Being on oxygen and trouble catching your breath
Patients can also lower the risk of exacerbation by doing the following:
- Following the treatment plan
- Take your medicine regularly
- Automate prescription refills
- Keep loved ones and friends informed
- Avoiding triggers
- Avoid tobacco smoke
- Quit smoking
- Household dust
- Pollution
- Getting vaccinated
- Flu or pneumonia vaccine
COPD Medications
COPD medicines help control symptoms and prevent serious health problems. Treatment eases symptoms, lowers risks, and slows the disease.
Your doctor may prescribe you to use:
- Short-acting bronchodilators (e.g., Albuterol): Bronchodilators open and loosen tight airways as quickly as possible when breathing becomes more difficult than usual. They can ease respiratory symptoms such as coughing and shortness of breath for four to six hours.
- Long-acting bronchodilators (e.g., Salmeterol): It helps keep airways relaxed for up to 12 hours. Regular use may lessen COPD flare-ups and assist in enhancing lung function.
- Corticosteroids (e.g. Budesonide): Steroid inhalers aid in decreasing the inflammation of the airways. They can also help reduce exacerbation.
- Antibiotics: Antibiotics kill the bacteria causing the infection (e.g., pneumonia) to prevent the worsening of COPD symptoms. Patients with COPD are more likely to develop more severe pneumonia, increased hospital admissions, and worse outcomes.
Apart from this regimen, Trelegy Ellipta is an inhaler used as a maintenance treatment for patients with moderate to severe COPD.
COPD makes daily tasks harder by causing breathing problems, mucus, wheezing, and chest tightness.
It is important to let your healthcare provider know if you experience these symptoms and stop smoking. Proper COPD care can enhance your functional abilities, exercise tolerance, and improve your quality of life, preventing potentially fatal complications associated with COPD.
References
Basics About COPD. 2023
COPD Causes and Risk Factors. 2024.
Four stages of COPD. 2024.